Table of contents
- Introduction
- Common appearances of lung metastases/lesions/nodules (Examples)
- Vanishing lesions (examples)
- Treatments
4.1. Radiation Treatments without fiducials
4.2. Radiation Treatments with fiducials
4.3. Afterloading
4.4. Brachytherapy - RFA (Radiofrequency Ablation) Treatment
5.1. Method images
5.2. RFA Results
5.3. Risk of pneumothorax - Scans with and without a tracer / contrast agent
- Fast growing nodule
- Ground-glass opacity (not metastases)
- Collapsed right lung and treatment result
- Your support, comments and critics
1. Introduction
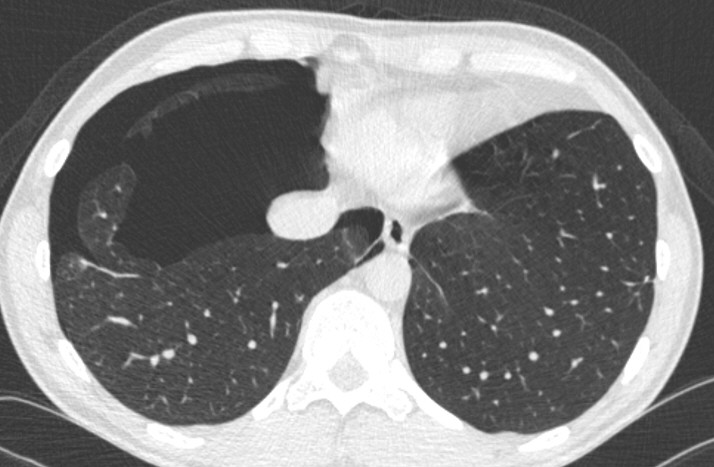
The following pictures show different lung scans from various ACC patients with lung metastases (focal rounded pulmonary opacities also called "nodules" or "lesions"). Most pictures are taken from a CT scan where a contrast agent was used. They show the different appearances of ACC lung mets. ACC has a tendency to spread to the lungs among other organs. ACC metastases are commonly random spread over the lobes of the lung.
A brightly lightened nodule seems to be faster growing than a greyish nodule. The white colour indicates a higher uptake of the tracer/ contrast agent. It seems that the brighter the nodule "shines" the more round it grows (probably high malignancy). Dark spots on the lesion are unclear. Shady lesions seem to be stable or slow growing (low malignancy). "Spready" lesions have a tendency to be stable, inactive or slowly growing. They might even decrease or vanish.
How to view my CT scans?
If your CD given by your radiologist with the CT pictures does not include a tool to watch them, a good choice is a freeware called UNIVIEWER that can be downloaded here: http://dicom.online.fr/fr/download.htm If you need to know how to use UNIVIEWER send us an email and ask for assistance.
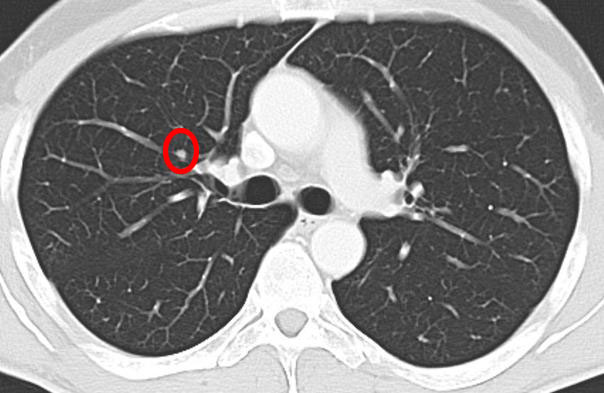
What do I see on the pictures?
A CT scan makes mirror images. The right side of the lung is on the left side on the picture. The clear white stripes, branches and spots are blood vessels. To see the difference between a blood vessel and a nodule you must scroll the pictures in the viewer frequently up and down many times. If it is a blood vessel, it will have a connection to the next picture level and fade out slowly in a blood vessel that appears as a branch. Metastases commonly "pop up" when you scroll up and down. Make sure that there is no equivalent blood vessel leading to it.
You are also able to see the different lobes. A very fine greyish outline is the border between two lobes. It takes some time to see clearly, but just be patient.
DISCLAIMER
NOTE: The comments and interpretations of what is shown on the pictures is what the patients were told by their radiologists. In many cases the interpretation has not been validated by a biopsy or by a surgery. The pictures of lung metastasis shall only give you an impression and overview of what you might see on your own CT scan pictures of the lung. The examples on this website might enable you to check your lung scans on your own and understand better the context for your physician’s comments.
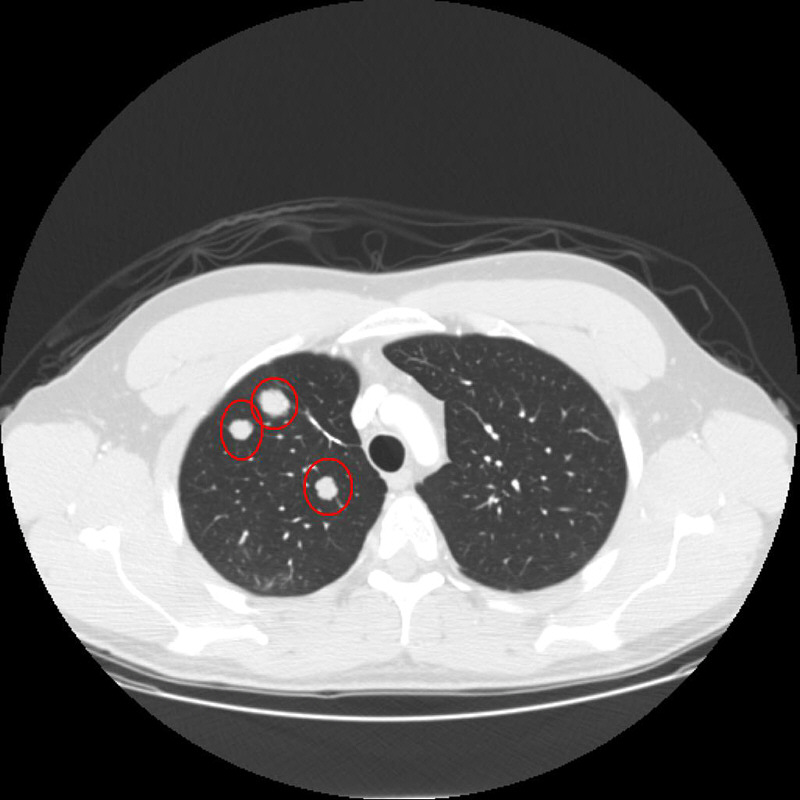
2. Common appearances of lung metastases/lesions/nodules (Examples)
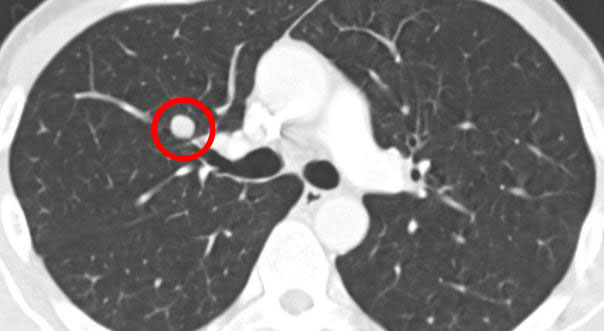
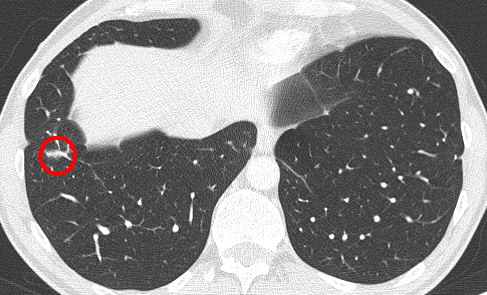
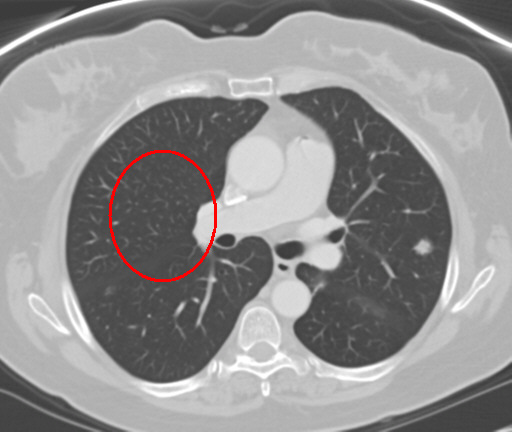
- A typical round shaped nodule, bright light:

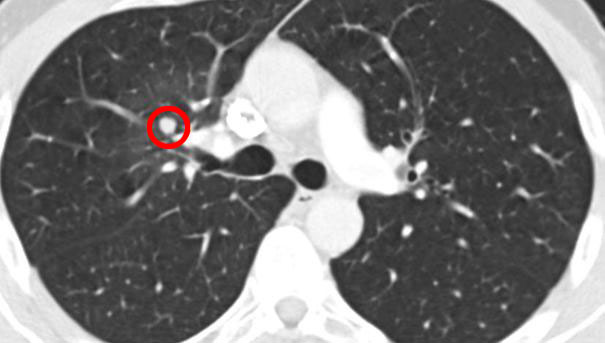
- Another round, solid, bright nodule
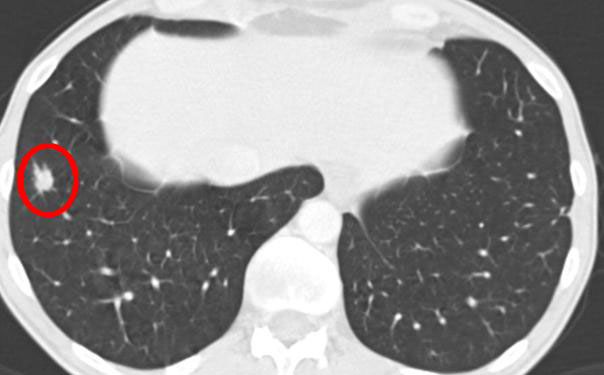
- ACC nodules / metastases with a greyish, non-solid, low alighted or shady appearance:
- A small hiding nodule with low brightness:

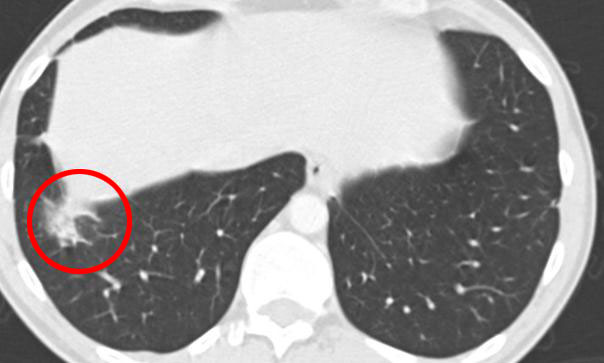
- Another shady, non-solid nodule:

- A lesion with dark spots or areas. It has been stable and unchanged for more than 18 months in the same patient as before, but started to decrease without any conventional treatment.

A very slow shrinkage can be seen and the dark areas get bigger:

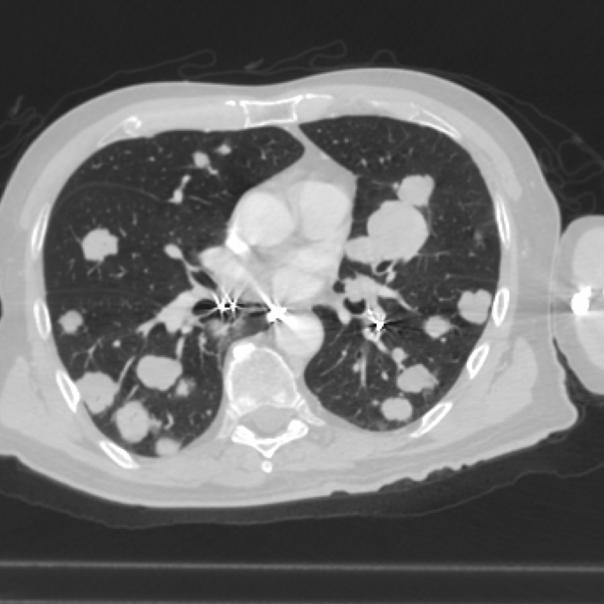
- The two following scans are examples of multiple lung mets. On the first picture you can count 19 mets. If a met grows very close to the chest wall it is likely to cause pain. On the first picture you can see several mets that grow very close to the chest wall:
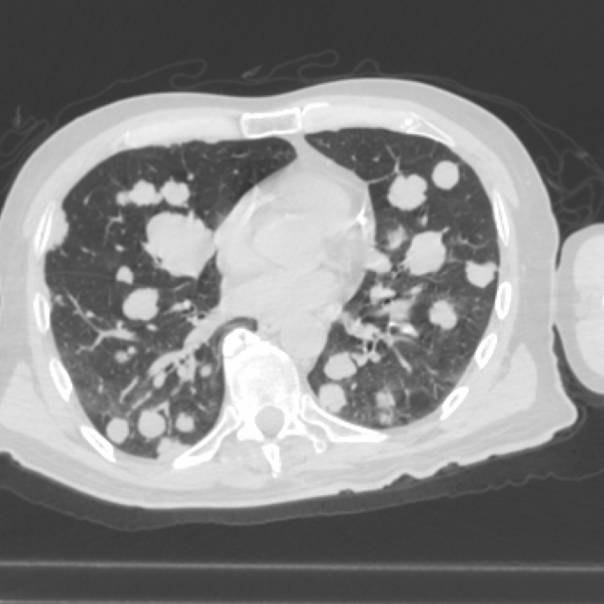
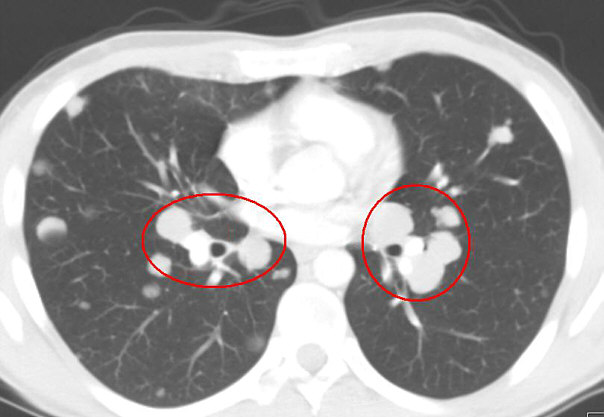
Here you can see some mets that are placed very close to the mayor airways and are suspicious to cause heavy breathing.
3. Vanishing lesions (examples)
An example of vanishing lesions without any conventional treatments over a period of 18 months.
In some cases spanning many cancer types, tumors gradually disappear without any medical treatment, either conventional or alternative. In other cases, these “spontaneous regressions” coincide with changed dietary practices and/or alternative treatments. Spontaneous regressions are not common, but have been documented (see Grillet 1984 and Kumar 2010).
The CT pictures below, provided by an ACC patient, appear to catalogue such a case. In this case, the patient travelled to a small Sri Lankan village for three months to be treated by a local doctor trained in traditional ayurvedic medicine (further informtion on ayurvedic medicine on Wikipedia). The treatment involved the institution of radical dietary changes for four months, including the elimination of proteins, reduced carbohydrates, Kasaya (a herbal decoction/tea), ayurvedic pills and plentiful organic green leaves and fresh vegetables. Meditation was also part of the treatment.
This picture was taken 18 months before:
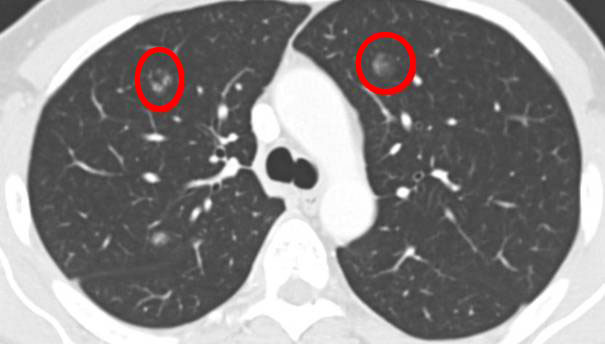
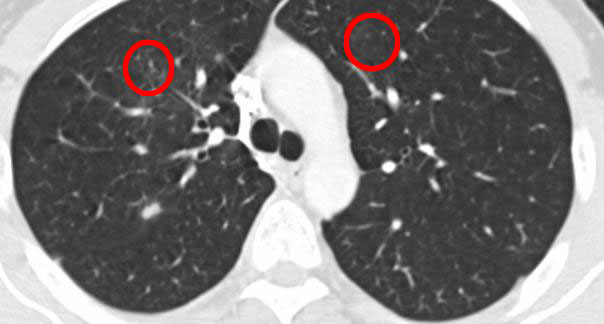
Same slice 6 months later (12 months before):

Another 6 months later (6 months before):

And another 6 months later:
4. Treatments
4.1. Radiation Treatments (SBRT: CyberKnife/Novalis TX/RapidArc) without fiducials (gold seeds to mark a position for a target of radiation)
- A nodule decreasing after a radiation treatment (before radiation):
3 months later after the SBRT with Novalis TX and RapidArc. The nodule has decreased in size and you can see a very slight shadow (light inflammation) around the radiated area caused by the radiation:
- Another nodule decreasing after a radiation treatment (before radiation):
3 months later after the SBRT with Novalis TX and RapidArc. The nodule has decreased in size and you can see a clear shadow (heavier inflammation) around the radiated area caused by the radiation:
12 months later after the SBRT with Novalis TX with RapidArc. The nodule has again decreased in size and the shadow showing heavy inflammation of the radiated area has gone.
- Another lesion before CyberKnife:
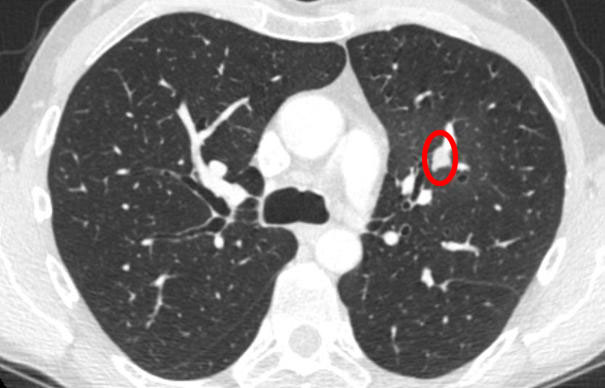
And the same lesion 6 months after the CyberKnife treatment. What you see is fibrotic scar tissue or an inflammation, that may occur after a SBRT treatment. It makes it difficult for the radiologist to follow up.

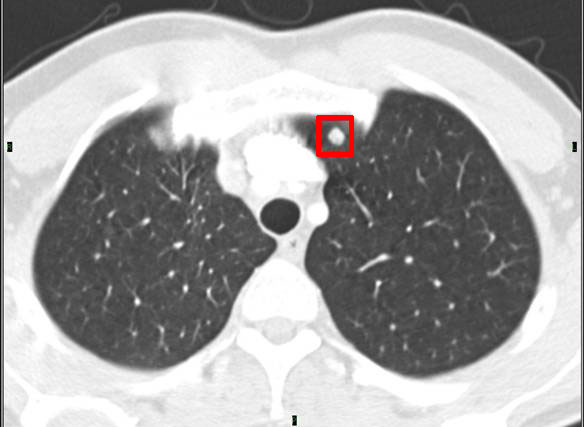
4.2. Radiation Treatments (SBRT: CyberKnife/Novalis TX/ with RapidArc) with fiducials
- Sometimes one or more fiducials are necessary to implant for a stereo tactical radiation (SBRT) e.g. CyberKnife, Novalis TX. You can see the reflections like from a bright star:

4.3. Afterloading
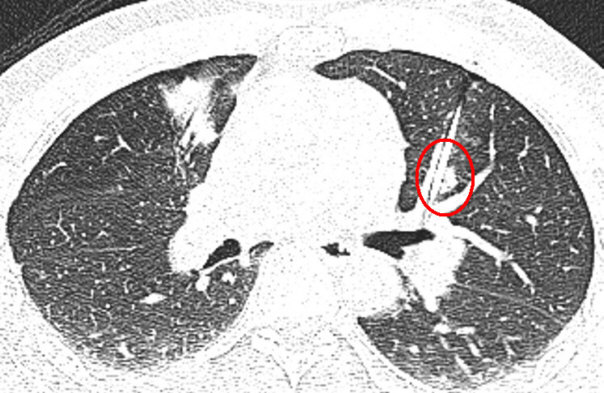
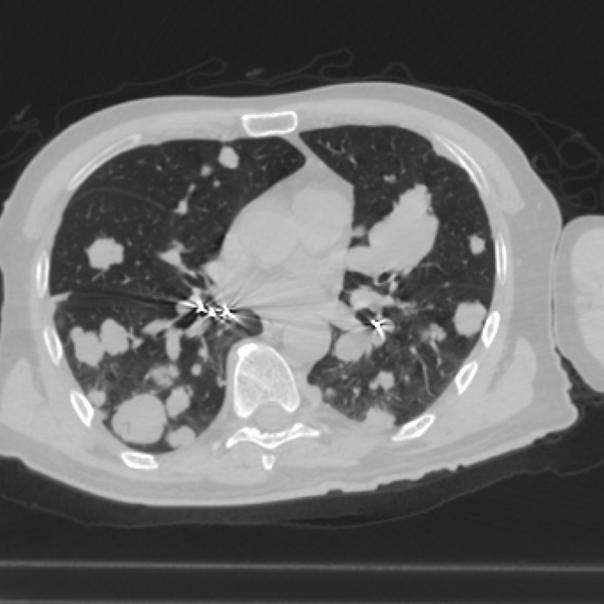
The next two pictures show a kind of hollow needle placed through the chest into a lung met. The needle is used for the afterloading technique which is a subtype of a brachytherapy and will be withdrawn after the radiation. The radiation is provided via the hollow core of the needle. One met is very close to the heart and the other is placed near an airway.

4.4. Brachytherapy
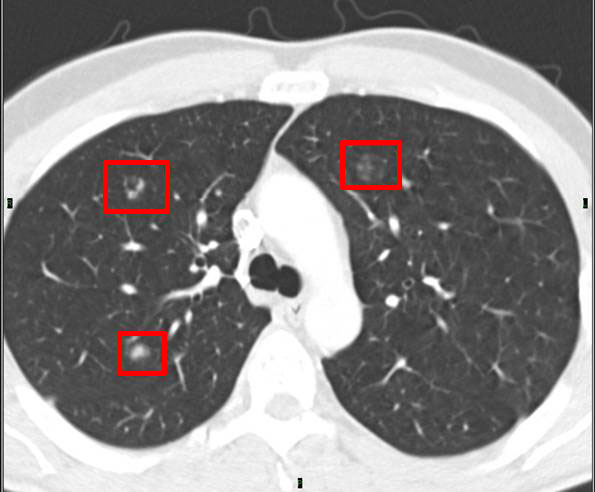
The following pictures show different stages of treated lung mets with Brachytherapy. The ACC patient had got three treatments of Brachytherapy for a total of 12 lung mets in December, 2010, in July, 2011 and the last one in March, 2012.
The first picture shows 3 lung mets shortly before any of the Brachytherapy treatments.
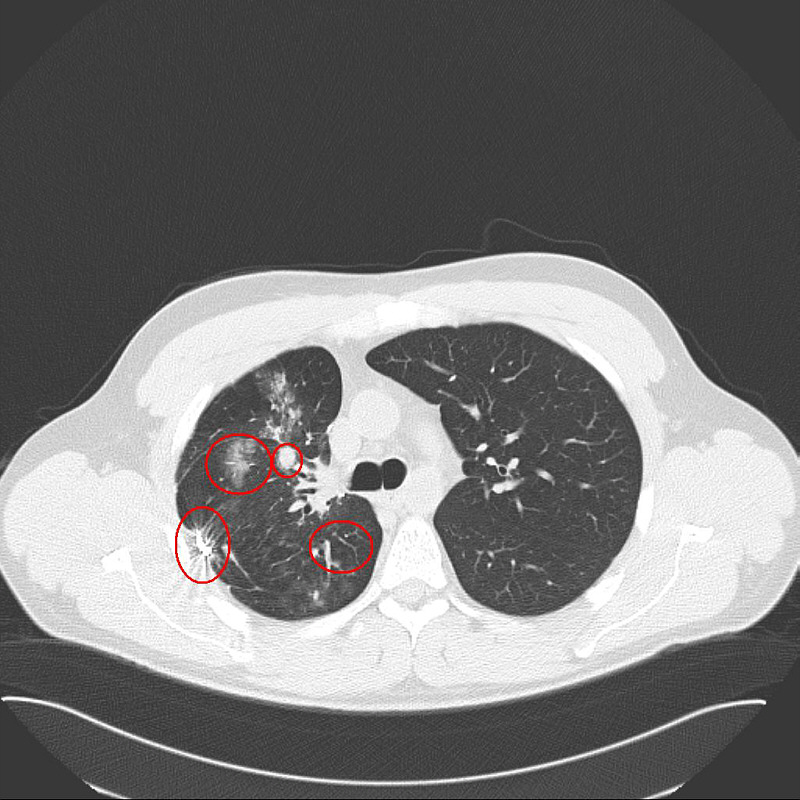
This picture was taken in March, 2012. It is difficult to see the shrinkage because the seeds show up so brightly, but none of the tumors are clearly visible any more.
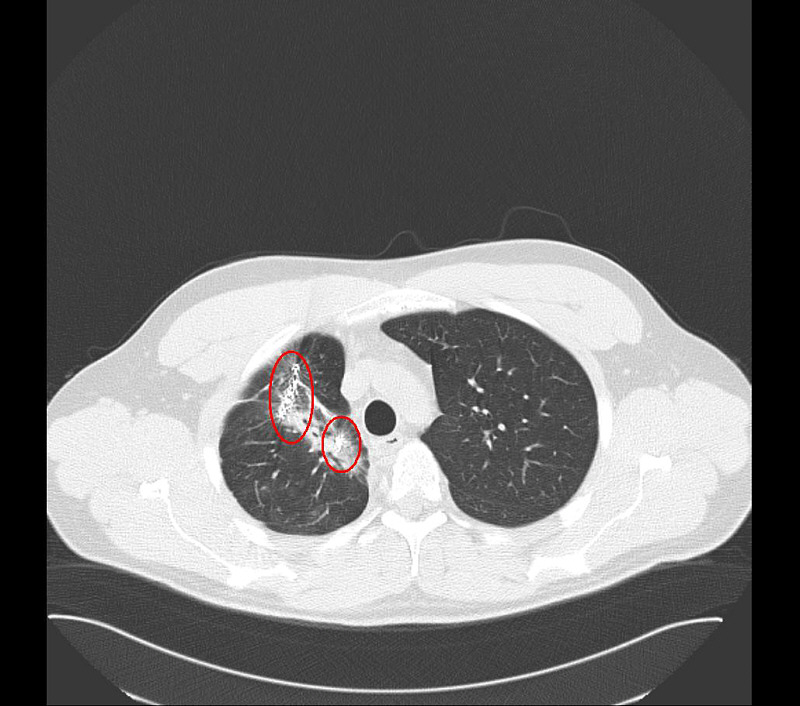
As another example the following picture shows four mets in different sizes of the same person from shortly before the Brachytherapy.
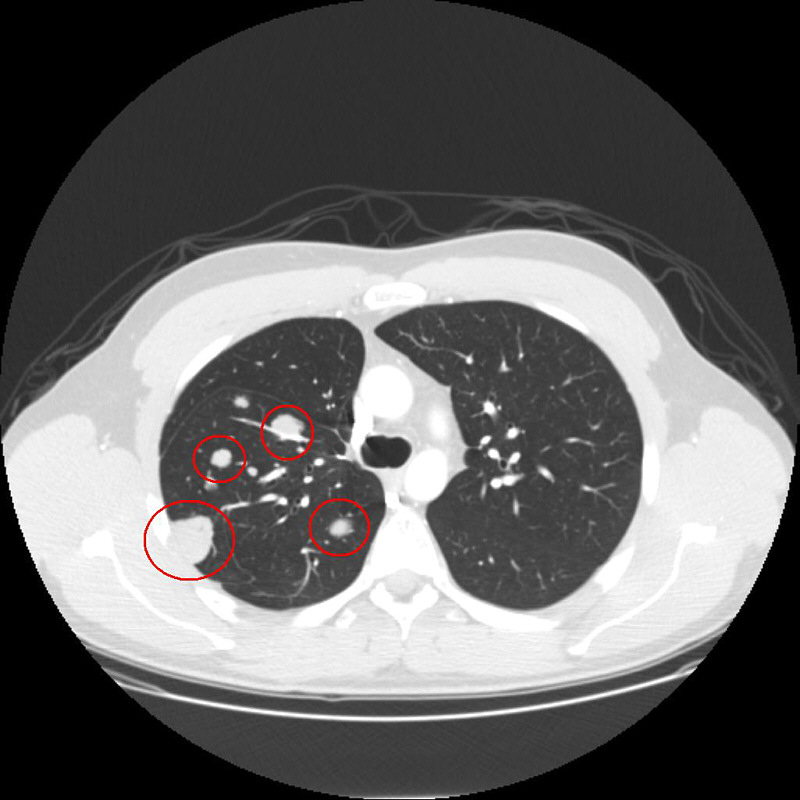
This picture was also taken in March, 2012. Here different stages of the shrinkage are clearly visible. The mets were treated on different times as mentioned before. Two mets have a complete regression (down right and upper left), one met that probably has been treated recently before the CT was done, has a little shrinkage (upper right) and the biggest met only shows the reflections of the implanted seeds (down left). The original size of the tumor is not visible any more.
5. RFA (Radiofrequency Ablation) Treatment
5.1. Method images
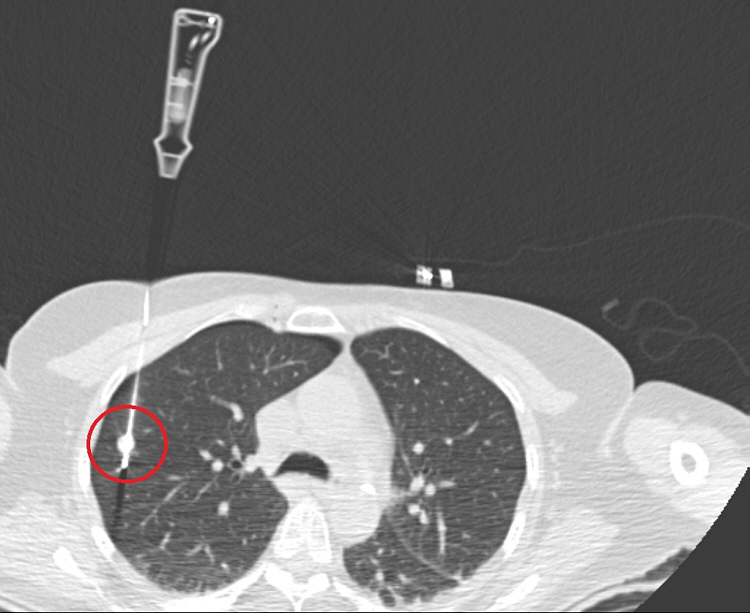
The next two pictures show a needle-like RFA probe that is placed through the chest inside the tumor. Commonly CT imaging is used for positioning. Once the probe is placed in the tumor, the radiofrequency energy is delivered. The radiofrequency waves passing increase the temperature within the met that results in destruction of the tumor. The needle will be withdrawn after the RFA.
Here you can see the top of the RFA probe like an array expanding (like an umbrella) after it is positioned in the tumor. The patient is lying on the front side.
5.2. RFA Results
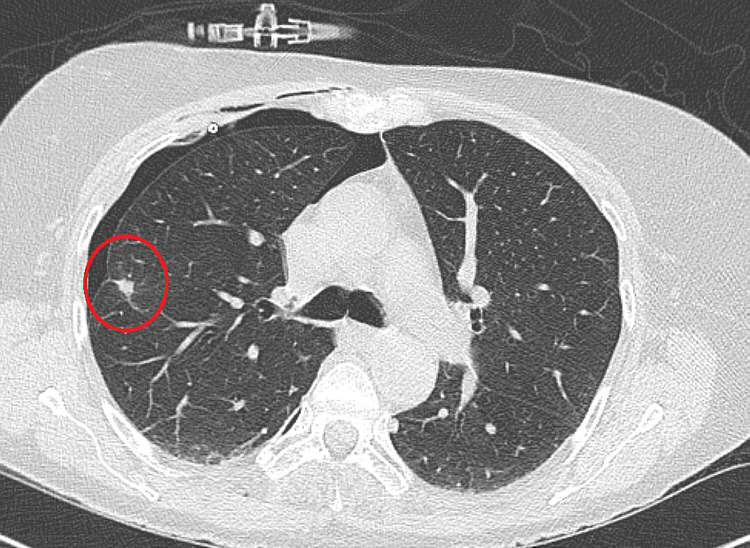
This image is taken nearly 6 months later; the patient is lying on the back side again during a normal CT. After 6 months it is very difficult to see if the cancer cells are dead. After a few months very often a met treated with RFA first seems to increase in size because of the scar tissue surrounding it. The dead tissue will shrink later and gradually be absorbed by the body and replaced with scar tissue. A long term follow-up is required.
These CT images show a met treated with RFA of another ACC patient. On the first image you can see the probe again hitting a met.
The second image was taken 6 weeks later. The ablation caused a larger size of the met because of the burning process.
The third image was taken 6 months after the RFA and shows a more greyish colour and a different, not round shape. The change in colour is most probably a sign of scar tissue. (Besides you can see a pneumothorax at the chest wall.)

5.3. Risk of pneumothorax
RFA, Brachytherapy and Afterloading have a common risk of pneumothorax (air getting into the chest cavity). The risk is similar to a CT guided lung biopsy procedure. This common complication is normally not serious and usually goes away on its own with no treatment. But even if the patient needs a chest tube to drain the air, the patient can go home after 1 or 2 days in hospital. You may experience some discomfort or pain in the treatment area for a few days and may also have a slight temperature and feel a bit tired and weak. Sometimes you will spit some blood for a few days. All this is not a serious complication though. Some other more rare side effects (e.g. bleeding, injury of a nearby organ, flu-like fever) may occur.
This image shows a more severe pneumothorax that needed a chest tube to drain the air. After one day it was almost gone again and the patient could leave the hospital.
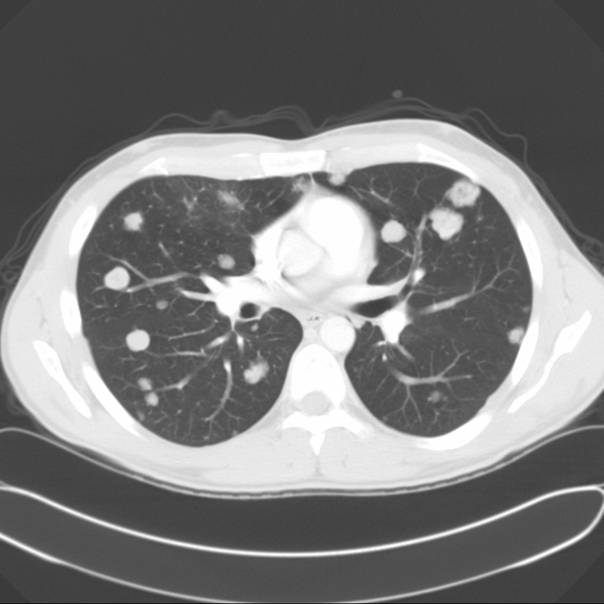
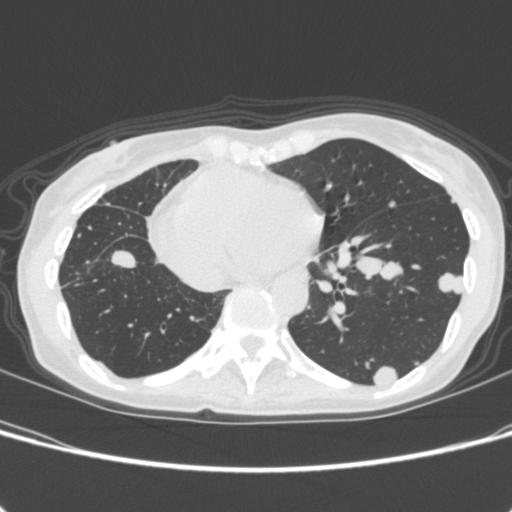
6. Scans with and without a tracer / contrast agent
- The following two pictures show a CT scan of the lungs with and without contrast agent. The difference is nothing of importance. The mets show up clearly in both pictures. This is the scan picture taken with contrast agent:
The following is the scan picture taken without contrast agent. The different look of the mets is just because of the slice. The width of slices might exactly be the same (normally between 2 mm and 5 mm), but the slice in another scan maybe in the space between two slices of the previous scan. To get the best follow-up you should chose slices with 2 or 3 mm space in between. In the following picture the width between the slices has been 5 mm:
7. Fast growing nodule
- An example of the development of a nodule with high malignancy / fast growth:
6 months later:

12 months later:

8. Ground-glass opacity (not metastases)
Ground-glass opacity is a non-specific term that refers to the presence of increased hazy opacity within the lungs that does not obscure the associated pulmonary vessels. It is a parenchymal abnormality and can reflect minimal thickening of the septal or it can be an alveolar wall inflammation or the presence of cells or fluid filling the air spaces, or a combination. If it is acute, it can represent pulmonary edema, pneumonia, or diffuse alveolar damage among others.
The following image is from a person with very few, small lung mets (ACC) and asthma/chronic bronchitis.
9. Collapsed right lung and treatment resul
The following picture shows a collapsed right lung which is visible as a bright white area where the right lung should be. (Remember that the left and right side are the opposite in a CT scan.) The reason for the extreme pneumothorax/lung collapse is not known. Some of the white spots are ACC nodules/mets.
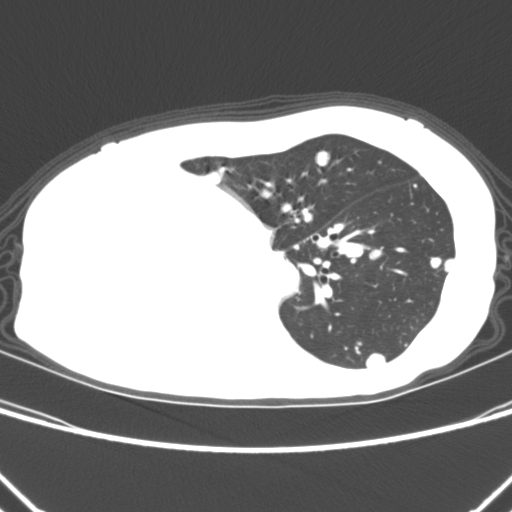
The second image shows the lung after a surgery more than one month later to save the right lung. The success has been permanent.
10. Your support, comments and critics
Your support is very important for this website. If you have other scans that could contribute to improve this website, please send an email to info@accoi.org We will respond and give you more details how to provide us with the pictures.
Comments and critics are always welcome, too.